In the aftermath of disasters, whether natural or human-caused, the immediate physical needs and safety of survivors understandably take priority. Nevertheless, the emotional and psychological toll disasters bring can be just as devastating, if not more so in the long run. Disaster mental health issues, though harder to see on the surface, require equal attention and care. Unaddressed trauma and emotional suffering take a steep psychological and social toll, impeding both recovery and rehabilitation efforts.
The Trauma and Stress of Disasters

Experiencing a disaster first-hand is incredibly traumatic and inflicts significant stress reactions. Survivors often struggle with overwhelming grief over lost loved ones and homes, anxiety about an uncertain future, difficulty sleeping and concentrating, intrusive memories and flashbacks of the traumatic event, and emotional numbness to cope.
Many develop depression, post-traumatic stress disorder (PTSD), and prolonged grief disorder in the months after. The rates of substance abuse also rise in affected communities. Children are especially vulnerable to long-term emotional damage without care and support. Their developing brains get stuck in a state of fear response even after immediate dangers pass.
Barriers to Mental Health Care Access
Unfortunately, several common barriers exist that limit disaster survivors’ access to quality mental health services and trauma support. Health infrastructure is often extensively damaged, while food and shelter take priority in rebuilding efforts. Few behavioral health professionals with trauma expertise live nearby, and securing funding remains a persistent challenge. Stigma surrounding mental illness and seeking counseling care persists among some cultures and communities as well, preventing many from pursuing treatment.
Potential Pitfalls of Short-Term Volunteer Efforts

Disaster relief organizations like Brother’s Brother Foundation rely on volunteers and missions groups that rotate in and out of sites across short durations. However, research shows this model has flaws when it comes to mental health support. Bonding quickly with survivors and then leaving soon after re-traumatizes them given attachments formed. It also precludes building local capacity when outside groups simply helicopter in with little collaboration or transfer of skills. Coordination between short-term response teams and long-term rebuild efforts rarely occurs. Follow up gets neglected.
Integrated, Multidisciplinary Approaches Recommended

Experts widely agree that collaborative and coordinated efforts between mental health professionals and relief organizations work best following disasters. Simply offering periodic counseling does not address trauma. Instead, psychosocial support services should integrate across sectors like health care, aid distribution lines, schools, and community development wile education, skill building, and counsel should be made readily available where survivors already gather for needs.
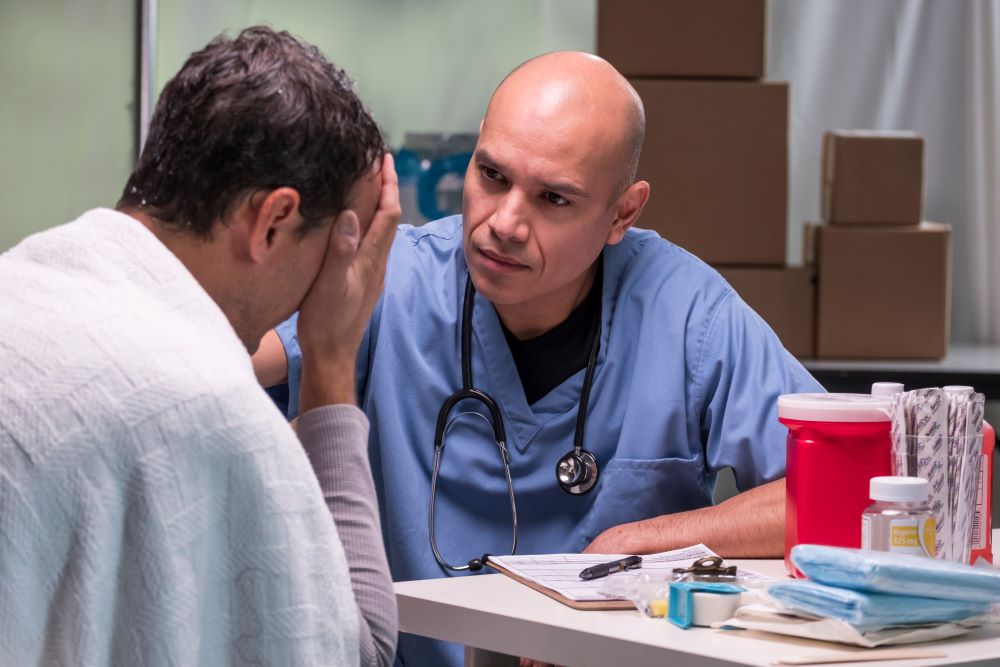
Deploying teams of psychiatrists, psychologists, and social workers from volunteer disaster mental health organizations to affected sites helps. They should rapidly assess needs and work alongside other medical services and rebuild efforts. Addressing trauma early fosters healthy coping strategies and resilience before issues compound. Ongoing support groups reduce isolation and normalize reactions. Creative arts therapies also show promise.
In communities that rely heavily on spiritual healers, collaborating with local religious leaders and traditional practitioners builds trust in counseling. Introducing concepts like self-care and stress management through a familiar lens helps lessen stigma. Support from other survivors proves equally valuable. Peer outreach workers carry credibility given shared backgrounds.
Conclusion
In the wake of disasters, grief and trauma counseling should be treated as essential as water, food, and shelter. Physical and emotional rebuilding go hand in hand toward community rehabilitation. Funding disaster mental health response equal to the priority given to infrastructure projects and recovery efforts means survivors’ inner wounds stand a better chance at lasting healing. With compassion, cultural understanding and evidence-based care, the suffering in trauma’s wake can give way to post-traumatic growth, resilience, and restored wellbeing over time.














